Reduced complication-related costs and enhanced patient recovery using the Ezisurg Endostapler
- owenhaskins
- Dec 16, 2024
- 4 min read
Bariatric and metabolic surgery (BMS) using the easyEndo™ Lite Endostapler (Ezisurg Medical) results in low rates of postoperative bleeding and leakage, highlighting Endostapler’s potential to improve the safety profile of laparoscopic techniques for managing morbid obesity, according to a study of 400 patients by researchers from King Hussein Medical Hospital, Amman, Jordan. The findings were reported in the paper, ‘The Risk of Leakage and Bleeding After Using the Ezisurg Endostapler Technique for Bariatric Surgery’, published in Cureus.

“These findings suggest clinical benefits, such as reduced complication-related costs and enhanced patient recovery. Incorporating advanced stapling devices like the Ezisurg endostapler may optimize bariatric surgical outcomes and streamline clinical workflows,” the researchers wrote. “Future multi-centre studies should focus on long-term outcomes, cost-effectiveness analyses and comparisons with alternative devices to strengthen the evidence base and inform clinical guidelines.”
easyEndo™ Lite Endostapler
According to the company, the easyEndo™ Lite Endostapler provides 120 articulation that allows a fully vertical cutting and suturing, which reduces the risk of postoperative leakage. The linear cutting stapler and its loading units are designed for the transection, resection and creation of anastomoses, and was approved by the FDA in 2021. The device features two triple-staggered rows of titanium staples, allowing for simultaneous tissue division along a central line. It is offered in three lengths - 260mm, 350mm and 440mm and five sizes to accommodate different tissue thicknesses (2mm, 2.5mm, 3.5mm, 3.8mm and 4.1mm). The device can be reloaded and fired up to 13 times during a single surgical procedure.
The company also claim that hardness of the knife blade been improved to reduce haemorrhage risk, far above industry standard, and the thinner fixed anvil allows for simple and easy insertion of narrow spaces, and the reduced size of the cartridge improves operation efficiency. Moreover, the device has been designed so it reduces tissue spillage during the firing process, thereby preventing tissue injury caused by over-pressing. In addition, the B-shaped formation achieve the best suture and haemostasis effect, speeding up the healing process by providing better blood perfusion. Finally, the device includes a double-release mechanism reducing the strain on the wrist and hands of surgeons, achieving one-handed operation.

In their retrospective single-centre study, the researcher sought to assess the prevalence of postoperative bleeding and leakage rates among patients undergoing laparoscopic bariatric surgery using the Ezisurg endostapler at the general surgery unit of King Hussein Medical Hospital, Amman, Jordan. They reviewed the medical records of 400 consecutive patients who underwent bariatric surgery at the facility between September 2023 and August 2024.
Patient data were retrieved retrospectively from the hospital's electronic database. Preoperative data collected included age, sex, BMI and procedure type. All procedures were performed by a single surgical team using the Ezisurg endostapler. In patients who underwent laparoscopic sleeve gastrectomy (LSG), four to six Ezisurg staplers with 60mm length cartridges were used. In patients who had laparoscopic Roux-en-Y gastric bypass (LRYGB), six to eight Ezisurg staplers with 60mm length cartridges were used.
Intraoperative assessment of leakage was conducted using CT scans with methylene blue test, while postoperative leakage was evaluated through Gastrografin testing and abdominal CT scans. Patients with tachycardia (pulse rate >100 beats per minute) were assessed for bleeding and were considered positive with a significant drop in haemoglobin for more than 3-5 g/dL according to Bleeding Academic Research Consortium (BARC) criteria. Patients with postoperative leakage were managed with laparoscopic gastroesophageal stenting or conversion to gastric bypass if necessary.
For those experiencing postoperative bleeding, some were treated conservatively, while others required surgical reoperation, targeting the trocar site or the stapler line. Vital signs and packed cell volume (PCV) levels were monitored postoperatively three times every 12 hours for patients with postoperative bleeding. Additional data on comorbidities, presence of gastroesophageal reflux disease (GERD), drainage during surgery, mean postoperative pain scores (using the Numeric Pain System (NPS)), time to first ambulation postoperatively and hospital stay duration were also recorded.
Outcomes
Of the 400 patients, 225 (80%) were female and the median cohort BMI was 43kg/m2. Patients underwent either LRYGB (n=135, 33.75%) or LSG (n=265, 66.25%). Medical comorbidities included diabetes mellitus in 72 (26%) patients, hypertension in 59 (21%) patients, and GERD in 40 (14%) patients. The median preoperative laboratory values for PCV and white blood cell (WBC) were 39% (36%, 42%) and 10 (8, 12.1)×109 cells/L, respectively.

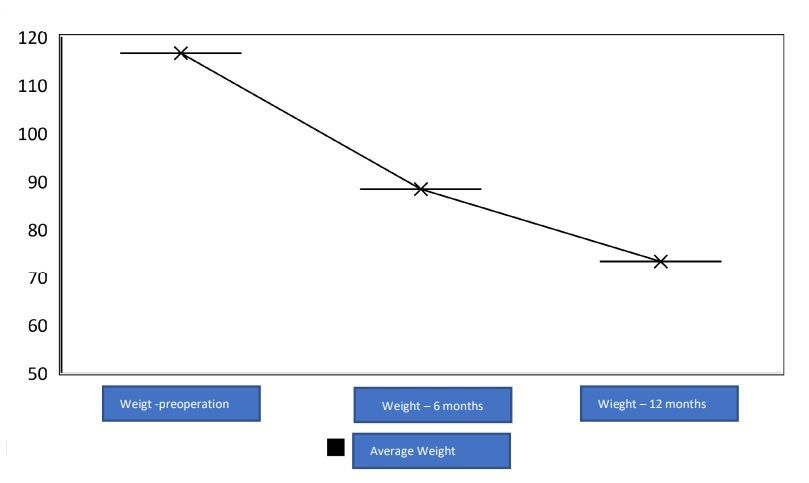
Complications occurred in ten (3.6%) patients, with three (0.75%) having postoperative leakage of which two were treated with laparoscopic gastroesophageal stenting and one patient was converted to gastric bypass (Table 1). Five (1.25%) patients had postoperative bleeding (Figure 1), of which two were treated conservatively and three required surgical reoperation two at the trocar site and one at the stapler line.

Median postoperative PCV and WBC values are 38% (35%, 42%) and 12 (10, 15)×109 cells/L, respectively. The median operation time was 96 (78, 134) minutes. All five patients with bleeding have received blood transfusion, and the median pain score was 3.85 (2.78, 5.57).
Patients who underwent LSG had a significantly higher rate of complications (8% vs. 1.1%; p=0.005), a longer duration time (median: 146 vs. 84; p<0.001), longer hospital stay (median: 9.1 vs. 5.9; p<0.001), and higher pain score (median: 6.20 vs. 3.07; p<0.001, Table 2).

“While our study highlights the safety and effectiveness of the Ezisurg endostapler, it is important to consider its broader clinical implications and limitations. The low complication rates could inform clinical decision-making and potentially shape guidelines for bariatric surgery,” the study’s authors concluded. “However, potential biases, such as selection bias from the single-centre design and the impact of operator experience, may limit the generalizability of these findings. Future studies should include diverse populations, multiple centres and varying surgical expertise to better evaluate the device's performance across different settings.”
To access this paper, please click here




Comments