The annual number of paediatric metabolic and bariatric surgery (MBS) procedures in the US more than doubled between 2010 and 2017, but Black And Hispanic teens accounted for a disproportionately low percentage of the procedures despite them having a higher prevalence of obesity than their white counterparts. The findings, 'National Trends in Pediatric Metabolic and Bariatric Surgery: 2010–2017', were published in the journal Pediatrics.
The study researchers, led by St Louis Children's Hospital-Washington University, sought to examine current US trends in paediatric bariatric surgery including procedure rates, procedure type, demographics, BMI, comorbidities, length of stay and complication rates, and primary payer. The researchers evaluated MBS utilisation rates among paediatric patients using weighted discharge data from 2010 to 2017.
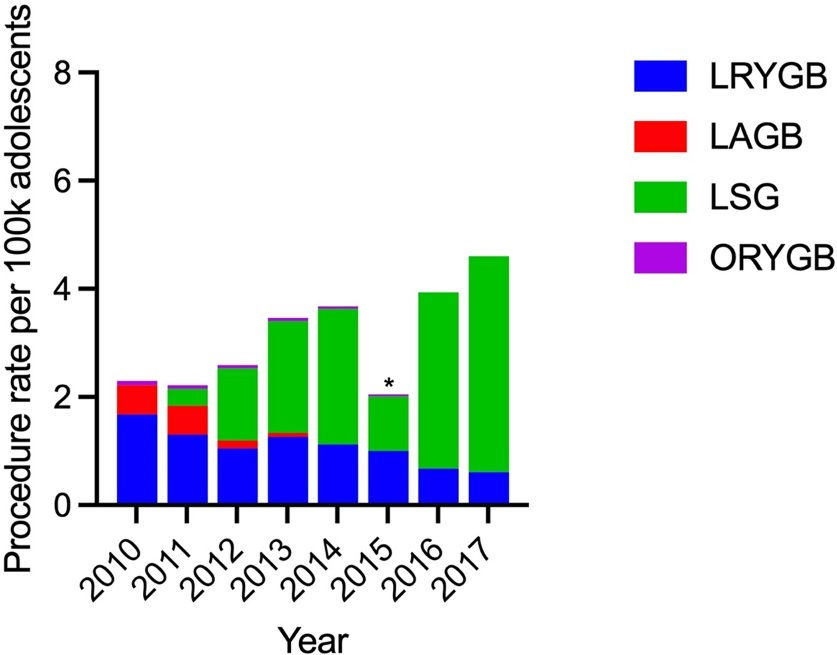
The study identified 9,014 index records and the overall annual procedure rates increased from 2.29 (1.62–2.96) to 4.62 (3.70–5.54) per 100 000 (p<0.001) between 2010 and 2017. From 2010 to 2017 (Figure 1), the type of procedure performed evolved with the rates of Roux-en-Y gastric bypass (RYGB) (1.68 [1.21–2.15] to 0.61 [0.42–0.80] procedures per 100 000; p=0.25) and adjustable gastric band (AGB) (0.53 [0.33–0.73] to 0.07 [0.01–0.13] per 100 000, p=0.17) decreasing, whereas sleeve gastrectomy (SG) increased significantly (0.31 [0.12–0.50] to 3.99 [3.33–4.65] procedures per 100 000; p<0.001). Unsurprisingly, the rate of open procedures was low and decreased over time (0.08 [0.00–0.16] to 0.045 [0.00–0.08] procedures per 100 000) and was too small to report after 2015.
The mean age did not differ significantly between 2010 and 2017 (18.10 [17.88–18.32] and 17.96 [17.70–18.22]; p=0.78), the cohort was predominantly female (76.5% to 75.4%, p=0.56). All racial groups showed an increase in the total number of procedures over time, however, although white children comprised 54.0% to 45.0% of the cohort from 2010 to 2017 (p=0.05) - the percentage of Black children undergoing MBS decreased over time from 18.2% to 14.6% (p=0.05), whereas numbers among Hispanic children saw a slight growth (17.2% to 25.9%, p=0.05). Insurance status was predominated by private payers (59.9% to 53.4%, p=0.06), though there was a trend toward increased proportions of Medicaid and Medicare increased from 24.5% to 36.3% (p=0.06) during the study period.
Between 2010 and 2017, the percentage of children with BMI greater than 50 grew from 4.2% to 16.2% (p<0.001). The only group to show the opposite trend was ‘morbidly obese’, which decreased from 48.4% to 17.2% over time. Hypertension (HTN) was the most common obesity-related comorbidity (21.2% to 16.2%), followed by obstructive sleep apnoea (20.3% to 25.0%), gastroesophageal reflux disease (16.2% to 24.6%), diabetes mellitus (15.2% to 11.3%) and nonalcoholic steatohepatitis (12.6% to 18.5%).
“Though a proven safe and effective weight loss intervention, paediatric MBS is underutilised with disproportionately lower rates among minority groups,” the authors concluded. “Further investigation into the racial and social determinants that limit access to MBS is essential to combat this growing public health crisis.”
To access this paper, please click here



Comentarios